Sick of Morning Sickness? Try These Pregnancy Nausea Remedies
Finding Relief from Pregnancy Nausea
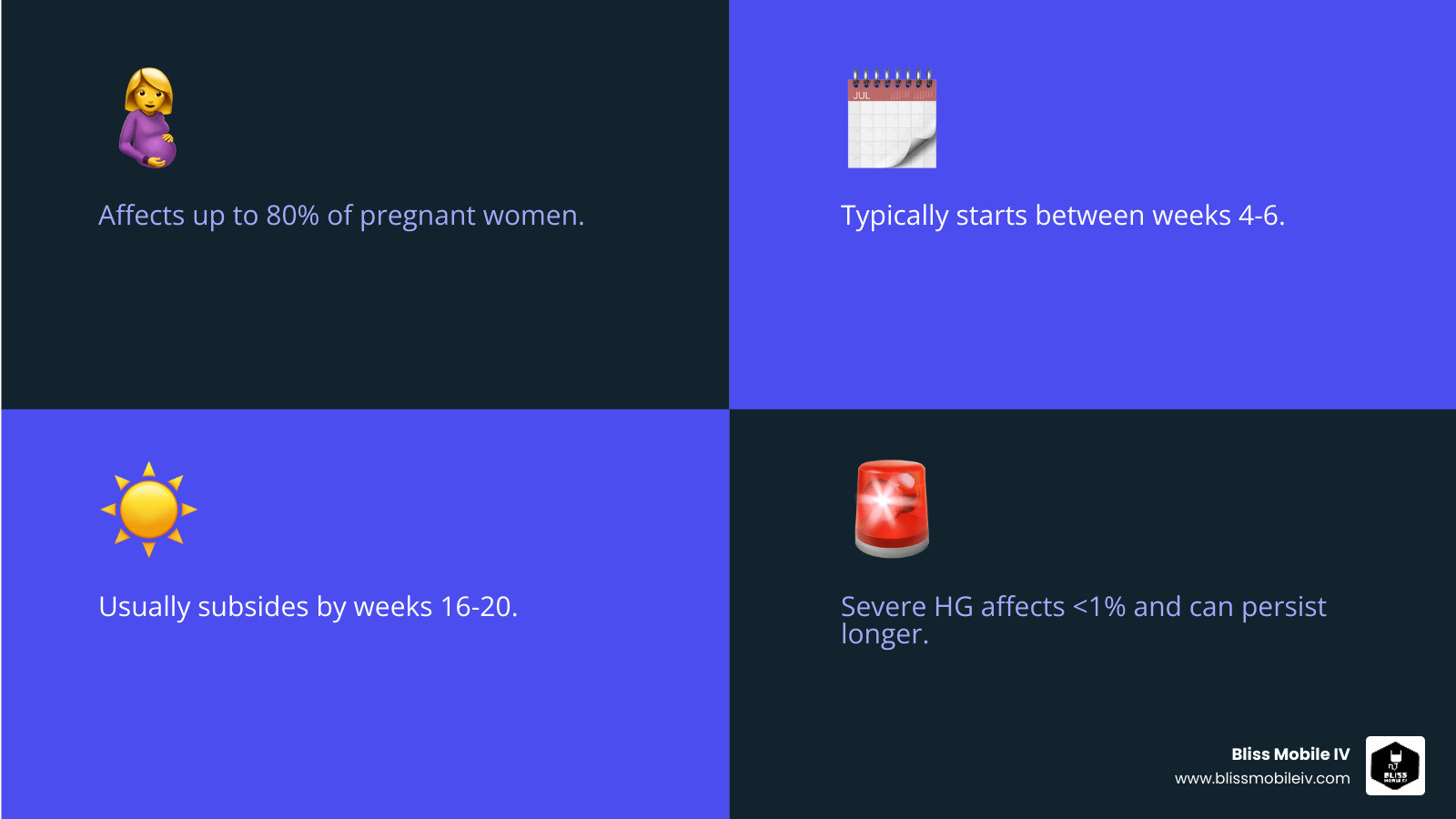
If you're searching for Pregnancy nausea relief, you're not alone. This common struggle, often called "morning sickness," affects up to 80% of expectant parents.
For quick relief, consider these strategies:
- Dietary Adjustments: Eat small, frequent meals, try bland foods, and incorporate ginger.
- Lifestyle Changes: Get plenty of rest and avoid strong smells or other triggers.
- Over-the-Counter Options: Discuss vitamin B6 or doxylamine with your doctor.
- Complementary Therapies: Explore acupressure or aromatherapy like lemon oil.
- Medical Help: For severe symptoms, a healthcare provider can discuss prescription medications or IV hydration.
Nausea and vomiting of pregnancy (NVP) can strike any time of day, typically starting between weeks 4 to 6. For most, it eases around week 14 and resolves by weeks 16 to 20. While challenging, typical NVP doesn't harm your baby, and many effective remedies are available, from simple lifestyle changes to medical support.
Understanding Morning Sickness: What It Is and Why It Happens
If you're feeling persistently queasy, gagging at familiar scents, or finding your daily life upended by waves of nausea, you're experiencing what's commonly known as "morning sickness." But what exactly causes this hallmark of early pregnancy?
While the precise mechanisms aren't fully understood, morning sickness is largely driven by the dramatic hormonal shifts that occur after conception. The primary culprit is thought to be human chorionic gonadotropin (hCG), the hormone detected in pregnancy tests. hCG levels rise rapidly in the first trimester, peaking around the same time morning sickness is often at its worst. It's believed that hCG directly stimulates a part of the brainstem known as the chemoreceptor trigger zone, or the nausea center. Surging levels of estrogen and progesterone also play a significant role. These hormones relax the muscles of the digestive tract, including the lower esophageal sphincter, which can lead to increased acid reflux. This slowing of the digestive process means food stays in the stomach longer, contributing to feelings of fullness and nausea.
Many pregnant individuals also experience a heightened sense of smell (hyperosmia), where once-neutral or pleasant scents—like coffee brewing, a partner's cologne, or cooking food—become overwhelming and trigger nausea. Your stomach also becomes more sensitive, reacting more strongly to certain foods, an empty belly, or even the pressure of a waistband. Some evolutionary biologists theorize that morning sickness developed as a protective mechanism, making the pregnant person averse to foods that could potentially contain toxins or parasites harmful to the developing fetus during its most vulnerable early stages.
Certain factors can increase your likelihood of experiencing nausea and vomiting of pregnancy (NVP):
- Multiple babies: Carrying twins, triplets, or more means higher levels of pregnancy hormones like hCG, often leading to more pronounced symptoms.
- History of motion sickness: If you're prone to feeling sick in cars, boats, or planes, your brain may be more sensitive to the hormonal signals that trigger nausea.
- Family history: Genetics may play a role. If your mother or sister had severe morning sickness, you have a higher chance of experiencing it too.
- History of migraines: Individuals who suffer from migraines often have a more sensitive neurological system, which may predispose them to NVP.
- First-time pregnancy: Sometimes, the body's first experience with the surge of pregnancy hormones can be more intense.
What are the symptoms?
Symptoms range from a constant, low-grade nausea to frequent vomiting. Strong food aversions are also common, where you suddenly can't stand the thought, sight, or smell of foods you previously enjoyed. Despite its name, morning sickness can strike at any time of day or night, and for many, it lasts all day. The severity varies dramatically, from a mild, manageable nuisance to a debilitating condition that significantly impacts your ability to work, care for other children, or perform daily tasks. The psychosocial impact can be substantial, leading to feelings of isolation, depression, and anxiety. It's crucial to acknowledge these challenges and seek effective Pregnancy nausea relief. Scientific research on the psychosocial impact of NVP highlights this often-overlooked aspect of the condition.
Is it a good sign?
While deeply unpleasant, there is a silver lining. Mild to moderate morning sickness is often associated with a lower risk of miscarriage. The same hormonal surges causing the nausea are also a sign of a healthy, robustly developing placenta. However, remember that the absence of nausea is also perfectly normal and is not a sign that anything is wrong. Every pregnancy is unique, and some individuals are simply less sensitive to the hormonal changes or are lucky enough to avoid morning sickness entirely.
Dietary and Lifestyle Tweaks for Nausea Relief
When battling pregnancy nausea, simple changes to your diet and daily routines can make a huge difference in finding Pregnancy nausea relief. The key is to be proactive and find what works for your body.

To manage nausea, the most important rule is to avoid an empty stomach. An empty stomach increases gastric acid, which can trigger queasiness. Instead of three large meals, adopt a grazing approach by eating small, frequent meals and snacks every 1.5 to 2 hours. This helps keep your blood sugar stable and prevents the deep hunger that can worsen nausea. A classic tip is to keep plain crackers, dry toast, or a handful of almonds by your bedside. Nibble on a few before you even sit up in the morning to get something in your stomach first thing.
Staying hydrated is also crucial, especially if you're vomiting. Dehydration can worsen nausea, creating a vicious cycle. If plain water is hard to stomach, try sipping cold, clear beverages like sparkling water, diluted fruit juice, or weak herbal tea. Some find that drinking through a straw helps. You can also try freezing juice or electrolyte drinks into ice pops for slow, soothing hydration.
Foods That Fight Nausea
Certain foods are more palatable and can help soothe your system. Focus on what sounds appealing, even if it's a limited menu for a few weeks.
- Bland Foods: The "BRAT" diet ( bananas, rice, applesauce, and toast) is a gentle starting point. Other easy-to-digest options include plain baked potatoes, simple broths, oatmeal, congee, pretzels, and plain pasta.
- Cold Foods: Cold or room-temperature foods often have less aroma and can be easier to stomach than hot, odorous meals. Try yogurt, cottage cheese, smoothies, fruit salads, watermelon, or a simple sandwich.
- Protein-Rich Snacks: Protein helps stabilize blood sugar and can keep nausea at bay for longer. Good choices include cheese sticks, nuts and seeds, hard-boiled eggs, Greek yogurt, or peanut butter on apple slices. Aim for around 60 grams of protein daily, spread throughout the day.
- Ginger, Lemon, and Peppermint: These three are nausea-fighting powerhouses. Ginger is a well-known remedy; try it in tea, chews, or real ginger ale. The scent of lemon can be incredibly refreshing—add a slice to your water or simply sniff a freshly cut lemon. Peppermint tea or sugar-free candies can also help settle a queasy stomach.
Foods and Smells to Avoid
Identifying and avoiding your personal triggers is key. Common culprits include spicy, greasy, fatty, or highly processed foods, as they are harder to digest and can irritate your stomach. Strong odors are a major trigger for many. The smell of cooking meat, garlic, onions, or brewing coffee can be overwhelming. If possible, open windows, use an exhaust fan, or ask a partner or friend to help with meal prep. Eating cold meals can also help you avoid cooking smells altogether.
Simple Lifestyle Adjustments
Your daily habits can significantly impact how you feel. Get plenty of rest, as fatigue is known to make nausea much worse. Aim for a full night's sleep and take naps during the day if you can. When you wake up, get out of bed slowly. Sit on the edge of the bed for a few minutes before standing up to avoid a sudden wave of dizziness or queasiness. Get fresh air daily by taking a short, gentle walk outside. The change of scenery and cool air can be very restorative. Wear loose, comfortable clothing that doesn't put pressure on your abdomen. Finally, if your prenatal vitamins seem to be making you sick, try taking them with a substantial snack or right before bed instead of on an empty stomach in the morning.
Natural and Complementary Therapies to Soothe Your Stomach
For those seeking gentle methods, many natural and complementary approaches can provide effective Pregnancy nausea relief. These methods are often a great first line of defense and can be used alongside other strategies to manage symptoms. It's always wise to consult your healthcare provider before trying a new therapy to ensure it's safe and appropriate for you and your baby.

The Power of Ginger
Ginger (Zingiber officinale) is one of the most well-researched natural remedies for nausea. Its active compounds, gingerols and shogaols, are believed to work by blocking serotonin receptors in the gut and exerting anti-emetic (anti-vomiting) effects on the central nervous system. A safe dosage is typically considered to be up to 1.5 grams of powdered ginger per day, often taken as 250 mg capsules four times a day. There are many other ways to incorporate ginger into your routine:
- Ginger tea: Steep fresh ginger slices or a tea bag in hot water.
- Crystallized ginger or ginger chews/candies
- Ginger ale: Look for brands made with real ginger for the best effect.
- Grated ginger: Add fresh, grated ginger to smoothies or soups.
Numerous scientific studies and reviews have confirmed ginger's effectiveness and safety for NVP.
Acupressure and Acupuncture
Acupressure is a traditional Chinese medicine technique that involves applying pressure to specific points on the body to alleviate symptoms. For nausea, the key spot is the Pericardium 6 (P6) or Neiguan point. To find it, place three fingers of your opposite hand across your inner wrist, starting at the crease. The P6 point is just below your index finger, between the two central tendons. You can apply firm, steady pressure to this point yourself for several minutes whenever you feel a wave of nausea. Alternatively, you can use acupressure wristbands, which have a plastic stud that applies continuous, gentle pressure to the P6 point.
While research on their effectiveness has produced mixed results, many people find these bands provide significant relief, and they are completely safe to try. For a more intensive and targeted treatment, acupuncture uses very fine, sterile needles on these same points and others on the body. If you consider acupuncture, it is essential to choose a licensed and qualified practitioner who has experience treating pregnant individuals.
Aromatherapy for Nausea
Given the heightened sense of smell in pregnancy, certain scents can be powerful tools for relief. Aromatherapy uses essential oils to help calm your stomach and mind. Simply inhaling a pleasant, soothing scent can make a surprising difference.
- Lemon Oil: The crisp, fresh scent of lemon is very effective. A study on lemon aromatherapy found it significantly reduced nausea and vomiting in pregnant women.
- Peppermint Oil: This invigorating scent can help settle a churning stomach and ease digestive discomfort.
- Spearmint Oil: A gentler alternative to peppermint, spearmint can also be very calming for the stomach.
- Lavender Oil: Known for its relaxing properties, lavender can help ease the stress and anxiety that may worsen nausea.
You can use essential oils by putting a few drops on a cotton ball or tissue to inhale, or by using an electronic diffuser. Always use essential oils with care during pregnancy. They are highly concentrated and should not be applied directly to the skin unless properly diluted and advised by an expert. Some oils are not safe for use during pregnancy, so always research or consult a professional.
Medical Options for Pregnancy Nausea Relief: From OTC to Prescription
When lifestyle changes and natural therapies aren't enough to provide adequate Pregnancy nausea relief, it's time to discuss medical options with your healthcare provider. Many safe and effective medications are available. Your doctor or midwife can help you weigh the benefits and risks for your specific situation to create a treatment plan that works for you.
Over-the-Counter Pregnancy Nausea Relief
Several effective over-the-counter (OTC) options are available, but it is essential to consult your doctor before starting any new medication, even one that doesn't require a prescription.
- Vitamin B6 (Pyridoxine): This is often recommended as a first-line treatment due to its effectiveness and high safety profile. A typical dose is 10-25 mg taken three to four times a day. It can be taken alone to manage mild nausea.
- Doxylamine Succinate: This is an antihistamine found in some over-the-counter sleep aids. It has been proven to be effective at reducing nausea. Because it can cause drowsiness, many providers recommend taking it at bedtime.
- Combination Therapy: The American College of Obstetricians and Gynecologists (ACOG) recommends combining Vitamin B6 and doxylamine as a highly effective first-line treatment. You can achieve this by taking the two separate OTC products, but it's crucial to do so under a doctor's supervision to ensure correct dosing and timing.
- Other Antihistamines: Other antihistamines like Diphenhydramine and Dimenhydrinate, often used for motion sickness, can also help with pregnancy nausea. However, they frequently cause significant drowsiness and should be used with caution and according to package directions.
Prescription-Strength Pregnancy Nausea Relief
For more persistent or severe nausea and vomiting that doesn't respond to OTC methods, your doctor might prescribe stronger medications. The goal is to find the lowest effective dose of a medication with a well-established safety record in pregnancy.
| Medication Name (Generic) | Form | How It Works | Common Considerations |
|---|---|---|---|
| Doxylamine-Pyridoxine | Oral tablet (extended-release) | This prescription-strength combination of an antihistamine (doxylamine) and vitamin B6 (pyridoxine) is a first-line standard of care. It works by blocking histamine receptors and replenishing B6 levels to reduce nausea. | This combination has been extensively studied and is considered very safe and effective. Dosing usually starts with two tablets at bedtime and can be increased as needed under a provider's guidance. |
| Metoclopramide | Oral tablet, IV, IM | A dopamine antagonist that helps by speeding up how quickly the stomach empties its contents and by blocking nausea signals in the brain. | A common dose is 5-10 mg orally, intravenously (IV), or intramuscularly (IM) every 6-8 hours. It can cause side effects like drowsiness, fatigue, and restlessness. Long-term use is generally avoided due to a small risk of a movement disorder called tardive dyskinesia. |
| Ondansetron | Oral tablet (dissolving), IV | A serotonin (5-HT3) receptor antagonist that is highly effective at stopping vomiting. It works by blocking the action of serotonin, a natural substance that can cause nausea and vomiting, in the brain and gut. | A common dose is 4 mg orally or IV every 8 hours, which can be increased to 8 mg. While very effective, some studies have suggested a small, increased risk of certain birth defects like oral clefts with first-trimester use. Therefore, a careful discussion with your doctor about the risks and benefits is essential. |
| Promethazine | Oral tablet, rectal suppository, IV, IM | A potent antihistamine with strong anti-nausea and sedative effects. It works on the brain's vomiting center. | A common dose is 12.5-25 mg orally or rectally every 4-6 hours. It can cause significant drowsiness, so it's important to avoid activities like driving. The suppository form can be very helpful if you are unable to keep oral medications down. |
| Corticosteroids(e.g., Methylprednisolone, Prednisone) | Oral tablet, IV | These powerful anti-inflammatory agents are typically used as a last resort for very severe, refractory cases of hyperemesis gravidarum that have not responded to other treatments. | Their use is reserved for the most severe cases due to potential maternal and fetal side effects with long-term use, such as glucose intolerance. They are usually prescribed by a specialist in a hospital setting. |
When Morning Sickness Becomes Severe: Understanding Hyperemesis Gravidarum (HG)
For a small percentage of pregnant individuals (around 1-3%), nausea and vomiting escalate into a severe and relentless condition called Hyperemesis Gravidarum (HG). This is not just "bad morning sickness"; it is a serious medical condition characterized by intractable vomiting that prevents you from keeping down adequate food or liquids. This leads to dangerous complications like dehydration, significant weight loss(defined as more than 5% of pre-pregnancy body weight), electrolyte imbalances, and nutrient deficiencies. If you are vomiting multiple times a day, losing weight, and unable to stay hydrated, it is critical to contact your doctor immediately. HG requires prompt medical management to protect the health of both you and your baby.
Signs and Symptoms of Dehydration and HG
Dehydration is a primary and immediate concern with HG. Watch for these warning signs and seek medical attention if you experience them:
- Feeling dizzy, lightheaded, or fainting, especially when standing up.
- Infrequent urination (less than 4 times in 24 hours) or passing very dark, concentrated urine.
- A dry mouth, lips, and skin.
- Extreme fatigue, weakness, or confusion.
- A racing or pounding heart.
- Persistent thirst, though you may be unable to drink.
- Inability to keep any food or liquids down for more than 12 hours.
Your doctor will diagnose HG based on your symptoms, a physical exam, and lab tests that may show ketones in your urine (ketonuria), a sign your body is breaking down fat for energy, and abnormal electrolyte levels.
Treatment for Hyperemesis Gravidarum
Treating HG is a multi-faceted process that often requires a hospital stay, at least initially. The primary goals are to stop the vomiting, rehydrate the body, correct electrolyte and nutritional deficiencies, and provide emotional support.
Treatment for HG can include:
- Intravenous (IV) fluids: This is the first and most critical step. IV fluids deliver hydration, electrolytes, vitamins, and sometimes sugar (dextrose) directly into your bloodstream, bypassing the digestive system entirely.
- Thiamine (Vitamin B1) Supplementation: Thiamine is crucial and is often added to IV fluids to prevent a serious neurological complication called Wernicke's encephalopathy.
- Anti-nausea medications via IV or IM: Stronger anti-emetic medications (like those detailed in the previous section) are given intravenously or as an injection for faster and more effective Pregnancy nausea relief.
- Nutritional support: If vomiting persists despite treatment, nutritional support may be necessary. This can range from a nasogastric (NG) tube that delivers liquid nutrition to your stomach, to, in the most severe and prolonged cases, total parenteral nutrition (TPN), where nutrition is delivered entirely through a central IV line.
We understand how physically and emotionally isolating and traumatic a diagnosis of HG can be. Bliss Mobile IV provides at-home IV hydration services in Utah, offering a convenient and comfortable solution for managing HG symptoms without the stress of a hospital visit. Our mobile IV therapy can quickly replenish fluids, electrolytes, and vitamins under the guidance of your primary healthcare provider.
Frequently Asked Questions About Pregnancy Nausea
It's natural to have a lot of questions when you're feeling unwell during what is supposed to be a joyful time. Here are answers to some of the most common concerns about morning sickness.
Does morning sickness harm the baby?
For the vast majority of cases, mild to moderate morning sickness does not harm your baby. In fact, as mentioned earlier, it's often associated with a lower risk of miscarriage, suggesting a healthy, developing placenta. Your baby is incredibly resilient and is very efficient at taking the nutrients it needs from your body's reserves. The primary focus during this time is for you to stay hydrated and eat what you can, when you can. However, severe and untreated Hyperemesis Gravidarum (HG) can pose risks due to maternal dehydration, weight loss, and malnutrition, which can potentially affect fetal growth. This is why seeking prompt medical care for severe symptoms is so important.
How long does morning sickness last?
While every pregnancy is different, morning sickness tends to follow a typical timeline for most people:
- Starts: Usually between weeks 4 and 6 of pregnancy, often one of the very first signs.
- Peaks: Symptoms tend to be at their worst around week 9, when hCG hormone levels are at their highest.
- Improves: Most people begin to feel significant relief around week 14.
- Resolves: For about 80% of women, nausea and vomiting are gone by weeks 16 to 20.
While most find relief by the second trimester, a smaller percentage may experience symptoms that linger longer. For those with HG, symptoms can sometimes persist for the entire pregnancy.
When should I call my doctor about nausea?
While some nausea is normal, you should always feel comfortable reaching out to your healthcare provider. It's especially important to call if you experience any of the following:
- Signs of dehydration (dark urine, dizziness, inability to keep liquids down).
- Vomiting more than 2-3 times per day.
- Losing weight.
- Vomiting blood or material that looks like coffee grounds.
- Feeling severely weak, confused, or faint.
- Nausea or vomiting accompanied by fever or abdominal pain.
Trust your instincts. If you feel your symptoms are severe or are significantly impacting your quality of life, it's time to seek help.
Can I get pregnancy nausea relief in the second or third trimester?
Yes, it's possible to experience nausea later in pregnancy, and it's important to mention it to your provider. It could be a temporary return of morning sickness, but it can also be related to other issues. Acid reflux (GERD) is a common cause, as your growing uterus puts pressure on your stomach, forcing acid up into the esophagus. In other cases, new or returning nausea can sometimes be a symptom of other conditions that need to be ruled out, such as a urinary tract infection (UTI), gallbladder issues, or even preeclampsia(if accompanied by other signs like high blood pressure or headache). Your provider can help determine the cause and recommend the right Pregnancy nausea relief for your stage of pregnancy.
Conclusion
Navigating pregnancy nausea is challenging, but you have many options for Pregnancy nausea relief. From dietary changes like small, frequent meals and ginger to lifestyle adjustments and complementary therapies, simple strategies can offer significant comfort.
For more persistent symptoms, don't hesitate to discuss over-the-counter or prescription medications with your doctor. For severe cases like hyperemesis gravidarum (HG), medical support such as IV hydration is crucial.
Don't suffer in silence. Bliss Mobile IV understands how debilitating nausea can be. We provide convenient, at-home IV hydration services across Utah to help you feel better without leaving your home.









